How Does Therapy Help a Child With ADHD?
Discover how therapy helps children with ADHD build focus, manage behavior, and thrive. Learn effective approaches, what sessions involve, and how parents can support progress.


Key Takeaways
- Therapy helps children with ADHD by equipping them with strategies to manage symptoms, improve their behavior, and enhance their overall quality of life.
- The CDC recommends that children under age six who are diagnosed with ADHD are treated with behavioral therapy before being prescribed medication, because of the proven benefits for children with ADHD.
- While the number of sessions needed can vary, consistent participation, collaboration with the therapist, and a supportive environment can lead to meaningful improvements in behavior, relationships, and self-confidence.
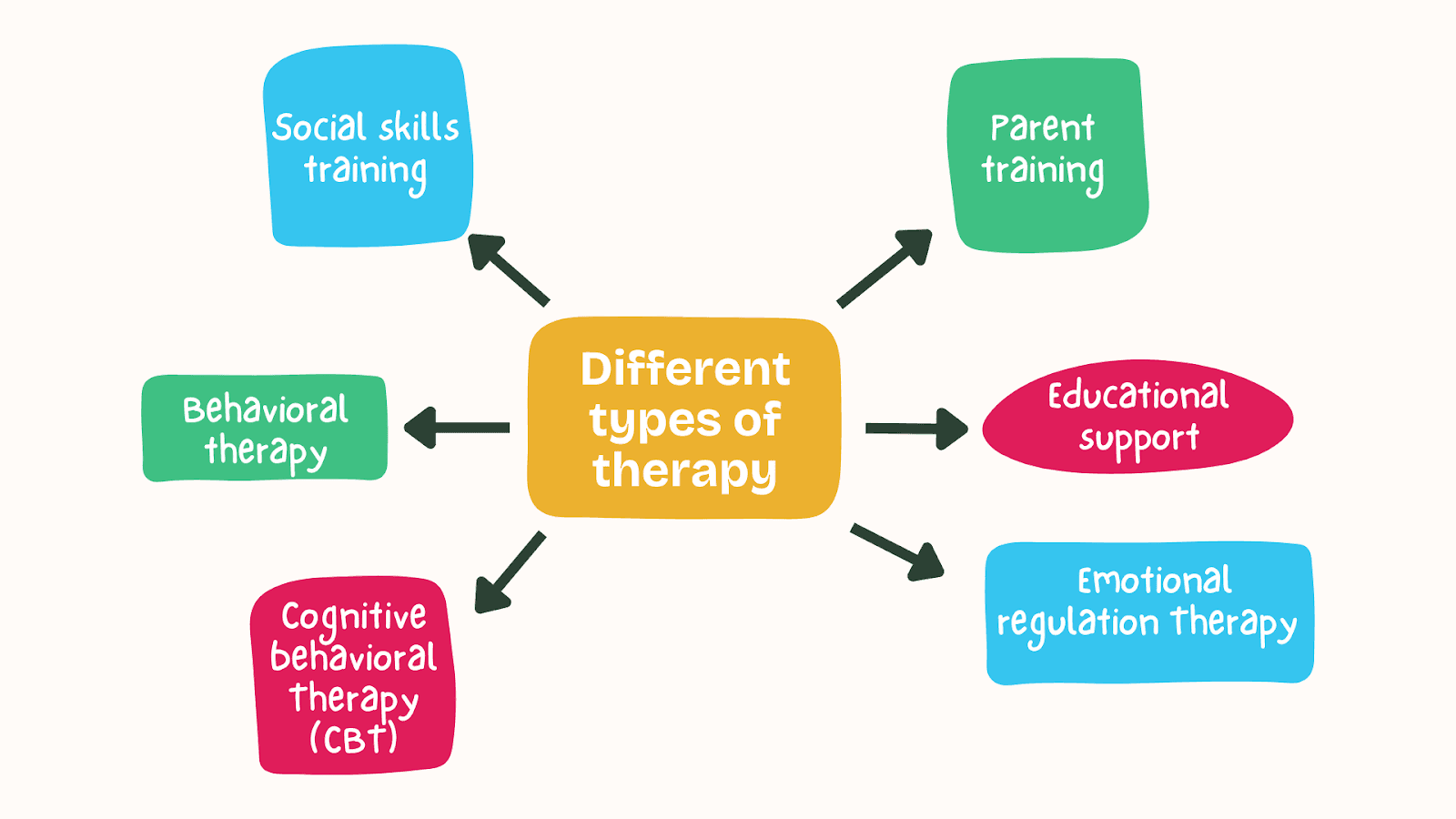
From behavioral techniques to parent training, various therapeutic approaches can help children develop skills and confidence.
This article is an in-depth overview of how therapy benefits children with ADHD, the different types of therapy available, and practical steps parents can take to support their child’s progress.
Does Therapy Help Children with ADHD?
Therapy can be highly effective in helping children with ADHD manage behaviors such as:
- Improving attention
- Reducing impulsivity
- Improving self-regulation
The CDC recommends that children under age six who are diagnosed with ADHD are treated with behavioral therapy before being prescribed medication, because of the proven benefits for children with ADHD.
For children over six, evidence supports a combination of behavioral therapy and FDA-approved ADHD medications (such as stimulants or non-stimulants). This multimodal approach has been shown to effectively manage ADHD symptoms, improving attention, focus, and behavior.
Different therapeutic approaches, such as behavioral therapy, play therapy, and family therapy, focus on teaching children practical skills to manage impulsivity, improve focus, and develop positive habits.
When combined with other treatments, such as medication or lifestyle changes, therapy supports children with ADHD to thrive academically, socially, and emotionally.
By addressing the root causes of disruptive behaviors and teaching coping mechanisms, therapy helps children build confidence and succeed in various areas of life.
Can Virtual Therapy Help Children with ADHD?
Virtual therapy can be a convenient and accessible way for children with ADHD to meet with a mental health professional.
Not only can online therapy be as effective as in-person sessions, but it also provides added benefits like the comfort of home, reduced stress from commuting, and greater consistency, which can lead to better long-term outcomes.
A review of six studies involving 261 ADHD patients (adults and children) found that online therapy significantly improved attention and social skills compared to no treatment. The findings highlighted a noticeable reduction in attention deficits and an overall improvement in social skills.

For children, being in a familiar and natural environment during therapy can help them feel more at ease, making it easier to engage in the process. This sense of comfort can minimize resistance, often seen when facing the stress of traveling to appointments, and supports a more seamless integration of therapeutic strategies into daily life.
Additionally, virtual therapy offers a practical solution for families who may otherwise struggle to access in-person care, ensuring children receive the support they need without unnecessary barriers.
How Does Therapy Help Children with ADHD?
Therapy offers children with ADHD strategies to manage symptoms, improve their behavior, and build life skills.
Different therapeutic approaches target specific challenges, such as impulsivity, inattentiveness, and difficulty regulating emotions.
Scientific studies have shown that therapy, often in combination with other treatments, can significantly enhance a child's academic, social, and emotional development. By focusing on individualized interventions, therapy helps children with ADHD thrive in various areas of life.
Behavioral Therapy
Behavioral therapy is one of the most effective treatments for children with ADHD.
It focuses on teaching children how to manage behaviors and build positive habits through reinforcement techniques.
Behavioral therapy also supports parents in implementing consistent behavior management strategies at home, creating a supportive environment for the child’s growth.
Common behavioral therapy tactics include:
- Positive reinforcement: Rewarding desired behaviors with praise, privileges, or tangible rewards encourages children to repeat those actions. For example, a reward chart can be used to track completed tasks or good behavior, offering a small prize for consistent effort.
- Consistent structure and routines: A clear, predictable daily routine helps children understand what’s expected of them. Consistency reduces anxiety and enhances focus. For example: Create a visual schedule for homework, meals, and playtime.
- Clear rules and expectations Setting specific, easy-to-follow rules helps children know what behaviors are acceptable. For example: Instead of saying, “Behave yourself,” provide instructions like, “Keep your hands to yourself, please.”
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a structured, evidence-based form of psychotherapy that helps individuals identify and change negative thought patterns and behaviors. It is based on the idea that thoughts, feelings, and behaviors are interconnected, and by addressing unhelpful thinking, individuals can improve their emotional well-being and develop healthier coping strategies.
CBT is widely used to treat a variety of conditions, including ADHD, anxiety, depression, and behavioral challenges. For children with ADHD, CBT focuses on skills such as managing impulsivity, improving organization, and regulating emotions. Sessions often involve goal-setting, problem-solving, and practicing new behaviors in real-life situations.
CBT helps children with ADHD identify and challenge negative thought patterns that influence their behavior.
By teaching practical skills like time management, problem-solving, and mindfulness, CBT equips children to manage symptoms such as impulsivity, disorganization, and negative thoughts.
A study on group CBT for ADHD found benefits in improving social skills, including empathy, assertiveness, and self-control, while reducing perceived difficulties in these areas.
Social Skills Training
It’s common for children with ADHD to have more difficulty with social interactions and making friends.
Social skills training is a form of behavioral therapy that teaches children how to communicate effectively, read social cues, and manage peer relationships.
Parent Training
Parent training equips caregivers of children with ADHD with tools to support their child’s development.
This includes strategies for managing challenging behaviors, setting clear expectations, and providing consistent reinforcement.
Research shows that parent training can improve a child’s behavior and reduce parental stress, creating a more harmonious family dynamic.
Educational Support
Educational support helps children with ADHD succeed academically.
Therapists work with educators and families to develop individualized education plans (IEPs) or 504 plans that provide accommodations such as extra time on tests, movement breaks, or modified assignments.
Studies show that combining educational support with other therapies can significantly enhance a child’s academic performance and self-esteem.
Emotional Regulation Therapy
Emotional regulation therapy helps children with ADHD manage intense emotions, such as frustration or anxiety, which can often lead to outbursts.
Techniques like mindfulness, relaxation exercises, and cognitive reframing teach children to respond to challenging situations calmly.
Research highlights that improved emotional regulation improves relationships and a stronger ability to handle daily stressors.
These therapy approaches, supported by evidence-based research, work together to address the multifaceted challenges of ADHD, fostering long-term success and well-being for children.
What to Expect in Child Therapy
Therapy for a child with ADHD is designed to address each child’s unique challenges and build essential life skills.
It involves collaboration between the child, their parents, and the therapist, often integrating teacher input if necessary.
Here’s what families can typically expect:
Initial Assessment
In an initial assessment, the therapist conducts an in-depth evaluation to understand the child’s specific symptoms, strengths, and areas of difficulty. This process often includes input from parents and, in some cases, teachers to create a complete picture of the child’s needs.
The information gathered during the assessment is essential for determining whether therapy is the right fit for the child.
It also helps the therapist develop a tailored treatment plan, including the recommended type of therapy, the proposed frequency of sessions, and specific goals to address the child’s unique challenges.
Parents and sometimes teachers may provide input to create a complete picture of the child’s needs.
Goal Setting
An important step in therapy for children with ADHD is establishing goals.
Examples of goals a therapist might set with children and their families include:
- Improve their relationships with parents, siblings, teachers, and friends
- Improve schoolwork performance, like completing class work or homework assignments
- Show a higher level of independence in self-care or homework
- Feel more self-confident
- Experience fewer disruptive behaviors
- Follow safety precautions while in the community or at school
Goals should be carefully designed to support your child’s growth and success. Effective goals are:
- Realistic: They should be achievable within a reasonable timeframe, considering your child’s current abilities and challenges.
- Specific and Actionable: Goals should focus on clear, tangible outcomes—things your child will be able to do or improve upon.
- Measurable: Goals should involve behaviors or skills that can be observed, tracked, and evaluated (e.g., using rating scales, progress charts, or other tools).
The therapist will structure the therapy sessions and strategies to help your child meet these targets, building on strengths and addressing areas of difficulty.
Clear and measurable goals also allow for tracking progress over time and adjusting the plan as needed to reach the best outcomes for your child.
Therapy Sessions
Sessions are typically interactive and tailored to the child’s developmental level.
Techniques like role-playing, modeling, and games may be used to teach skills such as impulse control, problem-solving, and emotional regulation.
Parent Involvement
Parents are often coached on behavior management strategies to reinforce therapy techniques at home.
Parent training may include guidance on setting clear rules, using positive reinforcement, and managing challenging behaviors.
From the very first session, parental involvement reaffirms therapy strategies are understood and reinforced at home.
- First Session Participation: Parents should be present and actively involved in the initial therapy session. This allows the therapist to gather insights about the child’s behaviors, challenges, and family dynamics while allowing parents to ask questions and understand the proposed treatment approach.
- 1:1 Parent-Therapist Sessions: Parents can schedule individual sessions with the therapist to discuss their child’s progress, address concerns, and learn specific parenting strategies. These sessions offer a chance to dive deeper into techniques for managing ADHD-related challenges, improving communication, and fostering positive behaviors.
- Behavior Management Coaching: Therapy often includes parent training to help families create a consistent and supportive environment at home. Parents are guided on effective behavior management strategies, such as:
- Setting clear and consistent rules
- Using positive reinforcement to encourage desired behaviors
- Addressing and redirecting challenging behaviors constructively
Progress Monitoring
Therapists track progress regularly, adjusting strategies to address the child’s evolving needs.
Families receive feedback on improvements and guidance on areas that need further support.
Progress is measured using clear and observable indicators, which may include:
- The child’s ability to identify and manage specific emotions (e.g., frustration, anxiety).
- Behavioral improvements, such as reduced impulsivity or better organization.
- Progress toward personal goals set at the beginning of treatment (e.g., completing tasks independently or improving peer interactions).
- Feedback from the child, parents, and sometimes teachers about perceived changes.
Rather than focusing solely on individual sessions, therapists assess long-term patterns to understand what strategies are most effective.
By examining trends, such as consistent reductions in emotional outbursts or improvements in attention, therapists can refine the treatment plan to focus on what’s working while addressing areas that need further support.
A Supportive and Safe Environment
Therapy provides a safe, nonjudgmental space where children can practice new skills and gain confidence.
It helps build trust and empowers the child to navigate challenges more effectively.
Therapy for children with ADHD requires patience, consistency, and teamwork. Over time, families can expect to see meaningful improvements in the child’s behavior, relationships, and overall well-being.
How Long Does Therapy Take for Children with ADHD?
It’s common for a child to meet with a therapist once or twice a week for at least a few months.
However, the duration of therapy for children with ADHD is different depending on the child’s specific needs, their symptoms, and the goals of treatment.
- Several weeks: Some children benefit from just a few weeks (5-8, for example) of therapy, particularly when targeting specific skills like managing impulsivity or improving social interactions.
- Several months: In some cases, therapy may extend over several months to a year or more, especially when addressing broader issues like emotional regulation, academic challenges, or family dynamics.
- Ongoing support: Even after achieving initial goals, some children may attend occasional follow-up sessions to maintain progress and address new challenges.
Progress depends on consistent participation, the child’s readiness to learn, and the support they receive at home and school.
How Can I Support My Child with ADHD While They’re in Therapy?
Providing the right level of support to your child while they’re in therapy is important for their success. There are several things you can do to help them succeed:
Be Consistent
You can show consistency by reinforcing the strategies and skills your child learns in therapy at home. It’s important to maintain a structured routine to help them feel secure and focused.
Stay Involved
Attend therapy sessions or parent training programs to better understand the techniques being used while your child attends therapy.
Schedule time to communicate openly with the therapist about your child’s progress so you can help address any challenges or concerns that arise.
Encourage Practice
Create opportunities for your child to apply new skills, such as problem-solving or managing emotions, in real-life situations.
You can also use positive reinforcement to celebrate their efforts and successes.
Advocate for Educational Support
Work with teachers and school staff so your child has the resources they need, such as an Individualized Education Plan (IEP) or 504 Plan.
Be Patient
Understand that progress may take time and that setbacks are part of the process. Offer encouragement and remind your child that it’s okay to make mistakes as they learn.
Focus on Self-Care
Supporting a child with ADHD can be challenging, so prioritize your well-being to stay positive and patient.
Conclusion
Therapy offers children with ADHD a pathway to better manage their symptoms and navigate challenges in daily life.
With a combination of professional guidance, parental support, and individualized strategies, children can achieve long-term success both academically and socially.
By committing to therapy and fostering a collaborative approach, families can create a positive and empowering environment for children to thrive.
Find a Virtual Therapist for Your Child with Emora Health
Emora Health connects families with licensed therapists who specialize in ADHD and evidence-based treatments like behavioral therapy, CBT, and social skills training.
Emora Health emphasizes a holistic approach, addressing not only the child's ADHD symptoms but also the well-being of the entire family. By offering resources, counseling, and education, they help create a supportive environment where children can thrive.
- Behavioral Treatments for Kids With ADHD. (n.d.). Child Mind Institute. https://childmind.org/article/behavioral-treatments-kids-adhd
- Behavior Therapy First for Young Children With ADHD. (2023). Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/adhd/articles/behavior-therapy-first-young-children.html
- Conclusions on Online Interventions for ADHD. (2022). PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC9274127/#:~:text=Conclusions,face%2Dto%2Dface%20treatment.
- Children and Mental Health. (n.d.). National Institute of Mental Health (NIMH). https://www.nimh.nih.gov/health/publications/children-and-mental-health
- ADHD Treatment: Behavior Therapy and Beyond. (2023). Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/adhd/treatment/index.html#:~:text=children%20with%20ADHD.-,Behavior%20therapy%2C%20including%20training%20for%20parents,as%20a%20diagnosis%20is%20made.
- Behavior Therapy for ADHD. (2023). Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/adhd/treatment/behavior-therapy.html
- Consistency Is Key to Success. (n.d.). Individual Matters. https://individualmatters.org/consistency-is-key-to-success/
- ADHD Treatment Study in São Paulo. (2023). SciELO Brazil. https://www.scielo.br/j/prc/a/8RGx4kwqy6YSGGYMrmVs79H/?lang=en
- Results on ADHD Treatment Success Rates. (2010). PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC2921569/#:~:text=Results%20suggested%20that%2056%25%20of,2005b).
- ADHD Therapy Insights. (2011). PubMed. https://pubmed.ncbi.nlm.nih.gov/22161373/
- Emotional Regulation in ADHD. (2015). PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC4477835/#S15
- Managing Emotional Dysregulation in ADHD. (2024). American Psychological Association (APA). https://www.apa.org/monitor/2024/04/adhd-managing-emotion-dysregulation#:~:text=62%2C%20No.,adults%20living%20with%20the%20disorder.
- Understanding Testing, Assessment, and Measurement. (n.d.). American Psychological Association (APA). https://www.apa.org/topics/testing-assessment-measurement/understanding
- Treatment of ADHD and Related Disorders. (n.d.). HealthyChildren.org. https://www.healthychildren.org/English/health-issues/conditions/adhd/Pages/Treatment-of-ADHD-and-Related-Disorders.aspx#:~:text=Examples%20of%20target%20outcomes%20for%20children%20with%20ADHD%3A&text=Better%20schoolwork%20(e.g.%2C%20completing%20class,can%20get%20her%20work%20done
- Positive Reinforcement. (n.d.). Simply Psychology. https://www.simplypsychology.org/positive-reinforcement.html
- What Is an Individualized Education Plan? (n.d.). University of Washington. https://www.washington.edu/accesscomputing/what-individualized-education-plan
